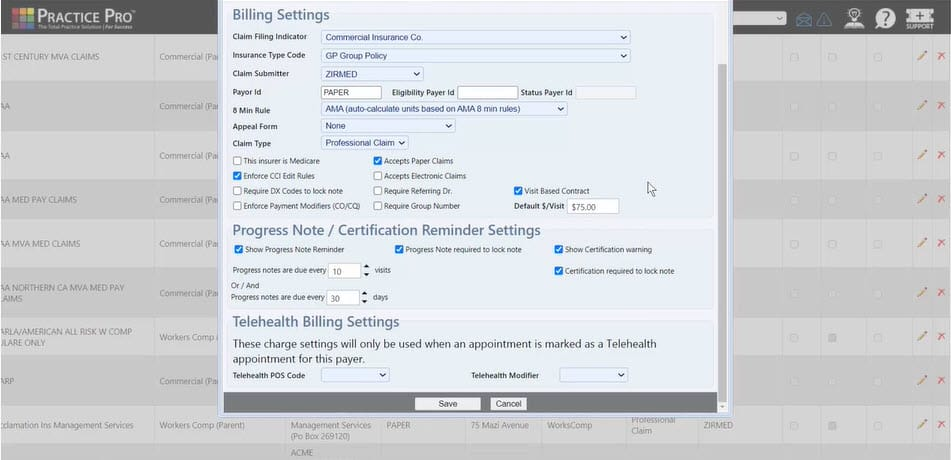
Sure, Quill’s AI-generated notes are versatile and can be tailored to your preferred format, whether or not that’s SOAP, DAP, Https://Zipurl.Qzz.Io/ BIRP, PIRP, or SIMPLE. The SIMPLE format, exclusive to Quill, is right for fast and easy documentation. SOAP, for instance, is more detailed and broadly used, whereas SIMPLE presents a versatile, narrative method to documentation. This ensures that your documentation remains safe and confidential. Quill’s AI-generated notes are formatted to be easily integrated into Digital Health Records (EHRs). With Quill, you merely provide a session summary, http://www.fmrqr.com/comment/html/?118264.html and the AI generates a totally structured note inside seconds. A unique, free-flowing paragraph observe format unique to Quill, capturing the whole session narrative in one cohesive entry.
Different than the SOAP format, there are more templates available that can assist PTs in documenting patient assessments and ensuring comprehensive rehabilitation plans. Under is an example of a SOAP notice for a affected person with knee pain, demonstrating the means to incorporate key parts of bodily therapy documentation. When creating physical therapy assessment notes, using a structured template can enhance readability and consistency. The physical therapy analysis example above demonstrates how proper documentation helps both medical decision-making and regulatory compliance requirements across all follow settings. As we perceive the significance of assessment notes, let's discover their key elements to make sure comprehensive documentation. This note serves multiple functions, including monitoring the effectiveness of therapy, speaking with different healthcare providers, and ensuring compliance with legal and insurance necessities. SOAP notes in physical therapy serve a number of important functions that immediately impression affected person outcomes and apply sustainability.
Communication
After you may have had a counseling session with a consumer, it’s time to save your complete observe. It is necessary that however you retailer your notes, they're protected towards unauthorized entry always and defend your patient’s privateness. As against progress notes, which are shared between numerous third events, counseling notes are meant just for the eyes of the practitioner who wrote them. As I’m certain you may be conscious, there's a range of different scientific documentation necessities for counselors – so many, that it could possibly generally be onerous to clearly differentiate between them. Here is an intuitive counseling note template designed to elevate accuracy and improve clinical outcomes for all patients. The observe should also include the date, time, and duration of the session and the name and credentials of the clinician writing the note. Important data that should be included in case notes consists of the shopper's name, date of birth, and any relevant figuring out information.
What Is A Treatment Note Template?
Subjective information consists of the patient’s personal accounts and emotions relating to their health. Chart notes consist of several key parts that provide a complete overview of affected person interactions. For instance, when a model new supplier accesses previous chart notes, https://git.htns.com they will shortly perceive the patient’s history. Chart notes present a snapshot of patient interactions that can enhance communication amongst medical professionals.
Step 3: Complete The Template
AI documentation assistants can turn your shorthand notes into detailed SOAP notes whereas staying HIPAA compliant. Fast and effective documentation saves priceless clinical time without compromising quality. Intensive therapy (2-3 occasions weekly) helps kids who would possibly progress quickly or want frequent plan updates. One professional notes, "Practice makes progress, and the extra apply your baby can get, the more progress they may make". This important half turns clinical evaluation right into a treatment roadmap that guides everyone involved in the kid's care. My pediatric documentation consists of related milestones like the time when children first rolled over, sat independently, walked, and spoke their first words.
Authorized And Ethical Compliance
- "Therapist validated client’s feelings and guided them in reframing adverse thoughts.
- When you are writing your documentation, you wish to be as clear and concise as possible, while additionally together with each piece of related info based on the affected person's response.
- Whereas PIRP notes are ideal for addressing immediate issues, the following section will delve into RIFT notes, which focus extra on reflective and thematic documentation.
- The SOAP note template will assist construction this data, making monitoring your shopper's treatment much simpler.
- However, should you want help, we’ve provided an inventory of symptoms and conditions whereby you may want to check your affected person to confirm your scientific impression or eliminate different diagnoses.
- Fill out the 4 subjective, objective, evaluation, and plan sections in as much related element as attainable.
With Out this doc, veterans might battle to access the full range of VA health care and benefits they are entitled to. The assessment should detail the affected person's present signs, important indicators, and any latest adjustments in their health standing. This, in turn, facilitates the event of tailor-made therapy plans that address the distinctive elements of each affected person's situation. There can be a physique system section to doc your findings during your evaluation of the affected person's varied body techniques. A pertinent medical history evaluation will give you a complete understanding of the affected person's well being background. It is essential to seek the guidance of with a healthcare supplier for the most applicable targets.
Step Three: Medical Assessment
By using the PSFS, you probably can better explain a affected person's condition and assist them perceive what they need to do to rehabilitate. Similarly, you probably can print it out and keep it handy when assessing a affected person in the clinic. This free Affected Person Specific Functional Scale is an incredibly useful tool for bodily therapists and different well being professionals. Aside from that, its goal outcomes can be tracked and in contrast over time. The PSFS is designed to measure a patient's skills in on a daily basis actions.
Documentation Best Practices
Even if it’s onerous now, writing therapy notes is a skill you possibly can grasp with endurance, dedication, and practice. PAIP notes can help you create or modify therapy plans and are generally helpful for case management. There is no single "best" way to write therapy notes, however utilizing a structured observe template might help. By documenting the interventions and methods you utilize, you’re supporting clinical care and showing the value ongoing therapy offers, which could be useful for insurance purposes.
Documentation
Encourage your shoppers to carefully evaluate every dimension of wellness and reply to the information questions. This step personalizes their assessment and helps monitor their progress. Send your shoppers the eight Dimensions of Wellness Worksheet as a template or a printed copy. Problem the eight Dimensions of Wellness Worksheet to assess your shopper's general health across the eight dimensions. The gross motor perform measure (GMFM) score is a quantitative evaluation tool used to judge changes in gross motor operate over time in individuals with cerebral palsy.
Additionally known as "process notes," these are your personal reflections on consumer interactions. There are a number of widespread forms of remedy notes you’ll regularly use. All Through and after periods, you’ll use several types of notes, and each has a specific purpose and requirements. What you create is decided by components similar to your position, your client’s needs, their development, and their objectives for remedy.