Periodontitis, a severe and progressive form of gum disease, affects millions of people worldwide. While many consider it simply an oral health problem, scientific research has consistently shown that periodontitis has far-reaching effects on the rest of the body. The mouth is a gateway to systemic health, and chronic inflammation or infection in the gums can influence and even exacerbate various medical conditions.
Understanding this connection is essential not only for patients but also for healthcare providers, public-health professionals, and even parts of the medical-supply industry, such as a mebendazole wholesaler who may interact with global health networks and recognize the importance of comprehensive wellness approaches.
What is Periodontitis?
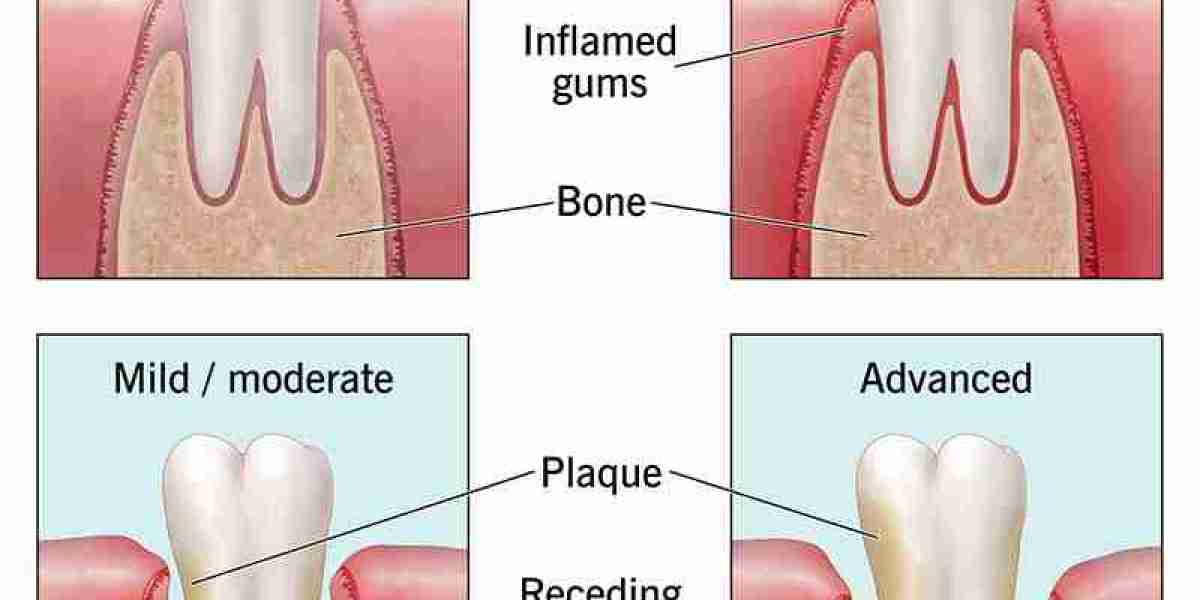
Periodontitis begins as gingivitis, a mild inflammation of the gums usually caused by the buildup of dental plaque a sticky biofilm made up of bacteria. If gingivitis is not treated, the inflammation can progress deeper into the tissues that support the teeth. Over time, the gums pull away from the teeth, forming pockets that harbor more bacteria. This leads to chronic infection, destruction of connective tissue, and eventually bone loss. If untreated, periodontitis can result in tooth mobility or tooth loss.
Symptoms include
Persistent bad breath
Red, swollen, or bleeding gums
Gum recession
Pain when chewing
Loose or shifting teeth
While poor oral hygiene is the main contributor, other factors increase risk: smoking, genetics, aging, stress, hormonal changes, certain medications, and underlying diseases like diabetes.
How Oral Health Connects to Overall Health
The mouth is closely linked to the rest of the body through blood vessels and the immune system. When harmful bacteria from periodontitis enter the bloodstream, they can trigger inflammation elsewhere, contributing to or worsening systemic diseases. Chronic inflammation is a core mechanism behind many health conditions, and periodontitis is one of the body's most common chronic inflammatory diseases.
Here are the key systemic connections:
1. Cardiovascular Disease
There is strong evidence that people with periodontitis have a higher risk of developing cardiovascular problems such as heart disease, stroke, and atherosclerosis. Researchers believe this happens through two primary pathways:
Inflammatory response: Periodontal bacteria stimulate chronic inflammation, which can contribute to plaque buildup in arteries.
Direct bacterial invasion: Certain oral bacteria have been found in arterial plaque, suggesting they can travel through the bloodstream and contribute to vascular damage.
Although treating gum disease alone does not guarantee prevention of heart disease, maintaining periodontal health significantly reduces one potential contributor to cardiovascular stress.
2. Diabetes and Blood Sugar Regulation
The relationship between diabetes and periodontitis is bidirectional each condition can worsen the other.
People with diabetes are more prone to infections, including gum disease, due to impaired immune response.
Periodontitis, in turn, makes blood sugar regulation more difficult by increasing systemic inflammation.
Studies show that treating periodontitis can improve glycemic control in diabetic patients. For individuals at risk for diabetes, oral health can serve as an early indicator of systemic problems.
3. Respiratory Problems
Bacteria from infected gums can be inhaled into the lungs, particularly in older adults or people with compromised immune systems. This raises the risk of:
Pneumonia
Chronic obstructive pulmonary disease (COPD) flare-ups
Respiratory infections in hospitalized patients
Good oral hygiene, therefore, plays a supportive role in respiratory health, especially for vulnerable populations.
4. Pregnancy Complications
Pregnant individuals with untreated periodontitis have a higher likelihood of experiencing complications such as:
Preterm birth
Low birth weight
Preeclampsia
Hormonal changes during pregnancy make gums more sensitive to plaque and bacteria, increasing the need for consistent oral care. Although periodontal therapy does not replace prenatal care, it is an essential part of a healthy pregnancy plan.
5. Rheumatoid Arthritis and Other Autoimmune Diseases
Chronic inflammation from periodontal bacteria may contribute to or worsen autoimmune conditions. For example, rheumatoid arthritis (RA) patients often have higher rates of periodontitis, and the severity of gum disease tends to correlate with RA flare-ups.
Some oral bacteria produce enzymes that may trigger autoimmune reactions in genetically susceptible individuals, demonstrating how tightly oral and systemic health are intertwined.
6. Oral Systemic Links in Public Health and Global Care
On a global health level, the link between oral and systemic diseases highlights the importance of integrated care. This perspective extends beyond clinicians to the broader healthcare supply chain. For example, a mebendazole wholesaler involved in distributing antiparasitic medications often collaborates with community health programs that address hygiene, sanitation, and disease prevention. Recognizing the interplay between oral health, infection control, and public health strategies helps create more holistic healthcare interventions, especially in underserved regions.
Periodontitis disproportionately affects low-income populations due to limited access to dental care, emphasizing the need for accessible prevention and education programs worldwide.
Preventing and Managing Periodontitis
The good news is that periodontitis is largely preventable and treatable, especially when detected early. Recommended strategies include:
Daily Habits
Brush at least twice a day with fluoride toothpaste
Floss or use interdental cleaners daily
Use antibacterial mouth rinses when recommended
Maintain a balanced diet rich in vitamins and minerals
Lifestyle Choices
Avoid smoking and tobacco use
Manage stress, which can weaken immune response
Monitor blood sugar if you have diabetes
Professional Care
Visit a dentist every 6 months for cleanings and exams
Seek periodontal evaluation if you notice persistent gum bleeding, swelling, or recession
Undergo scaling and root planing or other periodontal treatments when necessary
Professional intervention can halt disease progression, reduce pocket depths, and improve overall health outcomes.
Conclusion
Periodontitis is far more than a local mouth problem it is a chronic inflammatory condition with significant systemic implications. From cardiovascular disease and diabetes to respiratory illness and adverse pregnancy outcomes, the ripple effects of unchecked gum disease can be profound. Recognizing these connections helps individuals prioritize oral care as an essential component of whole-body wellness.
Whether you are a healthcare provider, a public-health professional, or even connected to the broader medical-supply chain such as a mebendazole wholesaler, understanding the importance of periodontal health contributes to a more integrated approach to global health. By combining good daily habits, regular dental care, and awareness of systemic links, individuals can protect both their smiles and their overall health.